Moderators
- Agathe Seguin-Givelet, MD PhD
Groupe Hospitalier Privé Ambroise Paré Hartmann, Neuilly-sur-Seine, France
- Stephen Cassivi, MD
Mayo Clinic, Rochester, USA
Presenters and Lectures
- Ilies Bouabdallah, Marseille, France
Protocols and practices to optimise minimally invasive surgery with digital chest drainage data
- Sebastien Gilbert, Ottawa, Canada
Optimising perioperative care and understanding the role of chest drains
- Kenji Suzuki, Kyoto, Japan
Maximising the benefits of minimally invasive thoracic surgery and ERAS, Japanese perspective
Thopaz+ is at the Center of Patient-Centered Care
Summary
A scientific symposium was held at the ESTS 2024 meeting in Barcelona, Spain, at which 3 prominent thoracic surgeons presented their unique perspectives on approaches to optimizing perioperative care for the lung resection patient.
Following introductory remarks by Stephen Cassivi, MD (Mayo Clinic; Rochester, Minnesota, USA) the first presenter was Ilies Bouabdallah, MD, Chief of the Department of Thoracic Surgery at Hôpital Saint Joseph (Marseille, France).
Protocols and practices to optimize minimally invasive surgery with digital chest drainage data
Likening surgery to a marathon that requires preparation, Dr. Bouabdallah provided an overview of how his institution uses ERAS principles to provide comprehensive perioperative care. He highlighted the importance of patient engagement in education, prehabilitation, measures to decrease psychological, physiological, and physical stress, and the importance of using minimally invasive techniques as well as 3D surgical pre-planning for personalizing the procedure. Postoperative measures included protecting the healing lungs by monitoring air flow and pleural pressure digitally, taking advantage of the portable nature of digital drain systems to enable early patient mobility, physiotherapy, and rehabilitation prior to discharge.
“As with any process, the success of an ERAS program requires preparation and planning. In our practice, digital monitoring of chest drains plays a role in enhanced recovery by protecting the lung by indicating and maintaining appropriate suction, and by enabling rapid patient mobilisation.” ︎
Optimising perioperative care and understanding the role of chest drains
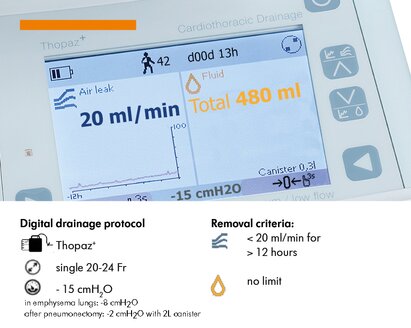
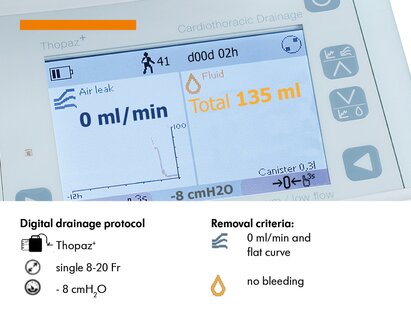
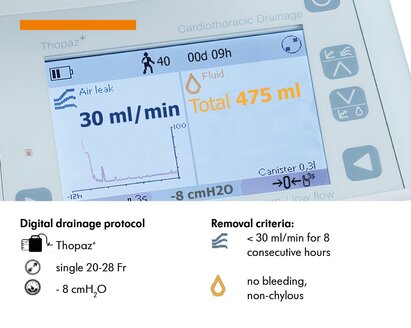
The next presentation was from Dr. Sebastien Gilbert, Professor of Surgery at the University of Ottawa (Canada). Dr. Gilbert’s particular interest is in applying process engineering, automation, and machine learning principles to harness the massive volume and variety of patient data that underlie an episode of care but currently go untapped. Pairing these principles and data with underutilized digital tools can foster the development of decision support systems for delivery of safe, efficient, high-quality care. Dr. Gilbert reviewed recent examples of studies that analyzed fluid volume and air leak data from digital drain systems to identify inflection points at which safety could be maximized while shortening chest tube duration.1, 2
“Going forward, quality improvement will require increasing synergy between humans and computers, with greater utilisation of the expertise and digital tools that are already available to us.”
Maximising the benefits of minimally invasive thoracic surgery and ERAS, a Japanese Perspective
After giving an overview of the evolution of lung resection surgery in the era of minimally invasive techniques and ERAS, Dr. Kenji Suzuki, Professor of Surgery at Juntendo University School of Medicine (Tokyo, Japan) presented the findings of several studies focused on the prognostic significance of preoperative exercise tolerance in patients with early-stage NSCLC.3 He then discussed the role of early chest drain removal and early mobilisation in enhanced recovery from lung resection, and presented studies showing that visualisation of air flow and pleural pressure over time, using digital drain data, can identify patterns that show when an air leak has resolved. 4 He also presented the results of a multicenter, randomised, controlled trial of early chest tube removal regardless of drainage volume,5 and his institution’s chest-tube management protocol based on his findings.
“Digital monitoring of airflow and pleural pressure over time is an objective way to visualise and recognise patterns that give us greater confidence when deciding it’s time to pull the chest tube.”
The presentations were followed by a productive discussion and a detailed Q&A session where attendees had the opportunity to obtain in-depth information directly from the speakers, facilitating a deeper understanding of the presented material.
The symposium was well-attended and fostered a rigorous exchange of ideas, elevating the scientific discourse among thoracic surgeons. Dr. Seguin-Givelet concluded it with a precise summary, highlighting how the integration of science is significantly enhancing postoperative patient care.