New ERAS (Enhanced Recovery After Surgery) guidelines are here, yet the manner in which they get rolled out in your institution is far less certain.
Thoracic surgeons lead the initiative. You establish best practices and protocols, based on data and experience. The patient stays within your care and within your control.
New ERAS (Enhanced Recovery After Surgery) guidelines are here1, yet the manner in which they get rolled out in your institution is far less certain. Consider these potential scenarios:
- Scenario 1:Administration leads the initiative. They interpret ERAS and institute mandatory processes and protocols for patients recovering after thoracic surgery.
- Scenario 2:Nurses lead the initiative. They determine how your patients will recover (and what kinds of outcomes they’ll have) and create guidelines for the rest of the care team.
- Scenario 3: Thoracic surgeons lead the initiative. You establish best practices and protocols, based on data and experience. The patient stays within your care and within your control.
Success, beyond the operation
Inclusion of a perioperative care program as part of an overall surgical program provides the best possible outcomes for patients.
Learn more about why the whole procedural package is often more important than the surgical technique by itself3.
For those patients for whom you choose to use external suction, here are the top 4 efforts to prioritise in perioperative fluid management so you can continue to shape patient recovery and stay on the cutting edge of care.1
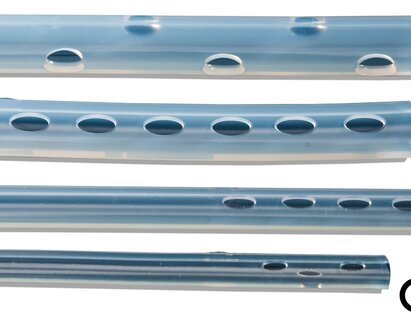
1. Use one chest drain (not two).
While this has not been shown to impact drainage or length of stay, using one chest drain enables earlier mobilization and reduces postoperative pain.3 Make this part of your protocol now to help you stay ahead of the curve.
2. Make 450 mL/day the threshold for removal.
Many institutions remove chest drains when patients reach 250mL/day. However, data show that there is no clinical difference between ≤450 mL/day and 250 mL/day thresholds.3,4
After thoracic surgery, establishing a 450mL/day threshold can get patients home sooner, without sacrificing quality.4
3. Use a portable drainage system to support early patient mobilisation.
ERAS protocols have been shown to reduce complications and Increase early discharge rates.
ERAS protocols that include early mobilisation have been shown to3:
- Reduce complication rates (6.6% vs 35%).
- Increase early discharge rates.
Mobilising patients sooner helps prevent many issues and streamlines recovery. Exploring strategies that promote mobilization, such as choosing drains that are portable, lightweight, and/or rechargeable, can be a key step.
4. Use a digital drain system.
Choosing a drain that uses a digital drain system like Thopaz+ will make it easier on your team and improve accuracy
The standard practice of “eyeballing the drainage canister” isn’t accurate enough for new ERAS protocols.4 Specific drainage thresholds require precise measurements.
Choosing a drain that uses a digital drain system like Thopaz+ will make it easier on your team and improve accuracy. A digital system can also improve tracking, monitoring during rehabilitation, and overall adherence.
Simple steps can put you ahead
Successful surgery starts with successful preparation. The same principle applies to managing guidelines for enhanced recovery after surgery.
Now is the time to manage your institution’s approach to new protocols by making sure that patient recovery stays in the hands of the thoracic surgeon.